Nan Witcomb was a well-loved friend of many in the WCH Foundation community. After passing away in November 2023 at the age of 95, Nan’s special connection and legacy of compassion – which started as a nurse trainee at the then Adelaide Children’s Hospital – will live on through a special gift left in her Will.
Nancy “Nan” Witcomb, born on 27 May 1928 in Adelaide, captivated hearts through her diverse endeavours, shaping her identity as a poet and storyteller under the pseudonym “Nanushka”.
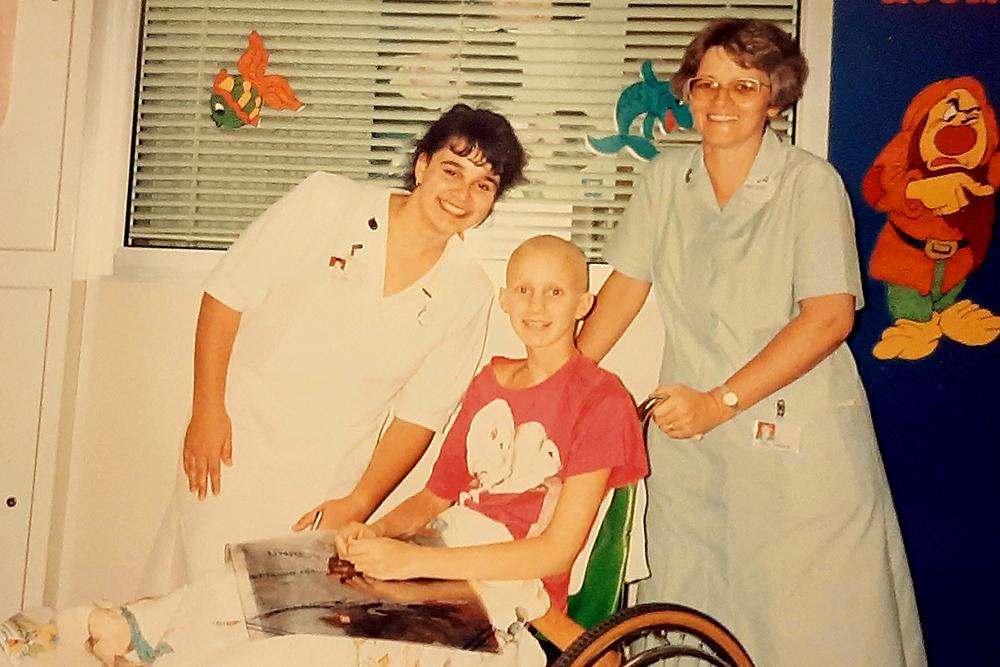
Nan’s lifelong connection with our Women’s and Children’s Hospital began after leaving the workforce at the Bank of Adelaide to pursue her passion for caring for others. She commenced her training as a nurse at the Adelaide Children’s Hospital and was later recognized with a Silver Cross medal for her dedication to nursing.
It has been said she loved her role as a children’s nurse, however her best friend Heather contracted polio. Whilst Nan cared for her until she passed, Nan felt she could no longer stay in nursing.
Nan’s life was marked by remarkable achievements and experiences. She was the sole woman on a flight to the atomic test area at Maralinga in 1956, the first woman interviewed on live TV in South Australia, and a writer for various comedy shows. Nan’s memoir, Up Here and Down There, chronicled her adventures as a senior regional hostess for Australian National Airlines (Ansett Australia), where she embarked on a 23-year career.
In the 1970s, Nan self-published her poetry and her work The Thoughts of Nanushka, which saw her gaining friends and fans worldwide. Her poem To Mourn Too Long for Those We Love resonated deeply, even being read at the funeral of INXS lead singer Michael Hutchence. Nan also ventured into radio hosting, captivating audiences with her warmth and wit on Adelaide AM station 5DN Cruise 1323.
Throughout her life, Nan’s bond with our Hospital remained as a regular attendee at many of our events with past nurses and other WCH Foundation donors. It is a special honour to now remember Nan and her legacy of compassion and support for others, knowing this spirit will live on through her wonderful Will gift.
To find out more about leaving a gift to the WCH Foundation in your Will, visit our bequest page.