Child and Family Health Service (CaFHS) provides a key role in the screening of infants and children at over 100 locations across South Australia, from Mount Gambier to Coober Pedy and everywhere in between.
The service completes approximately 11,000 preschool health and development checks each year, which is just over half of the cohort of four-year-old children in South Australia.
As part of the four year health and development checks, vision screening is imperative in identifying issues that are detectable and treatable. Early identification and treatment of eye and vision problems aims to optimise vision prior to starting school and reduces the likelihood of permanent vision loss.

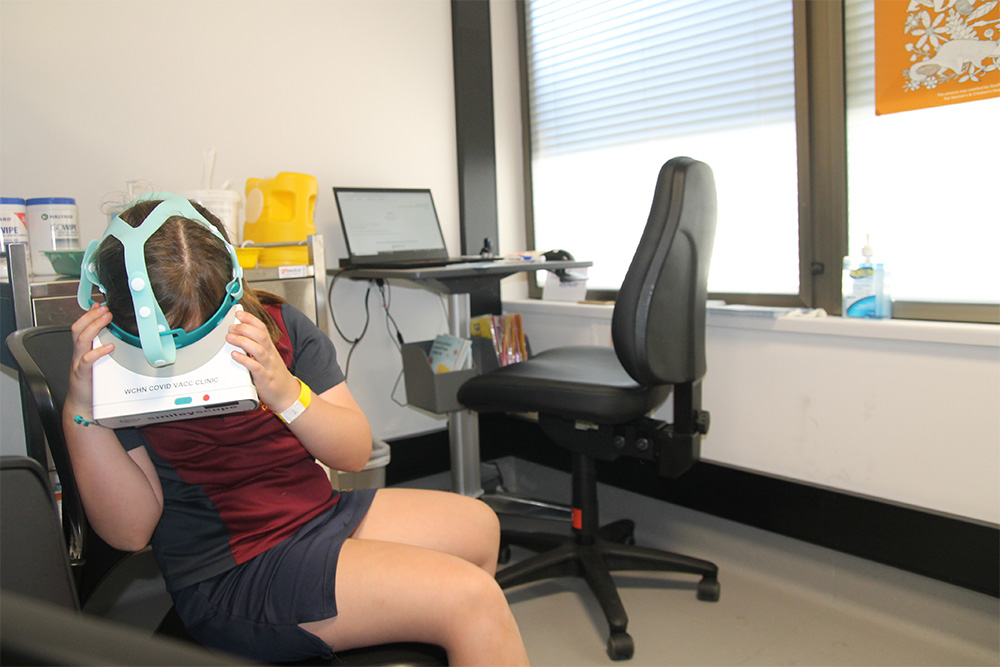
Ellora engaged in her vision screening test with a Kay Picture Test book.
We provided CaFHS with $18,000 to fund the purchase of 122 Kay Picture Test vision screening books – the ‘gold standard’ for vision assessment of four- to five-year-olds. Children engage in the fun ‘game’ of identifying the book’s pictures from a distance to test their eyesight during their preschool checks.
The books are significantly more user-friendly and age-appropriate than the previous charts used and are highly accurate and readily portable.
Four-year-old Ellora found the test lots of fun, making assessing her vision quick and easy!
Fiona Grant, CaFHS Acting Advanced Clinician, says, “The vision screening books will support a more user-friendly and best practice screening approach for the early detection of vision problems in young children.”
“This tool will support referral for further assessment and treatment if required before a child starts school and will positively impact their commencement in formal education.”

Ellora showing off this wonderful new tool for vision screening.