The commitment and passion of Bridget Claire McCartan for burns nursing continues to leave a lasting mark on the field, empowering dedicated nurses to advance their expertise and deliver exceptional care.
To honour her memory and tireless dedication, the Bridget Claire McCartan (BCM) Scholarship was established by Bridget’s family to support nurses committed to burns care, offering them opportunities for professional growth and fostering excellence within the specialty.
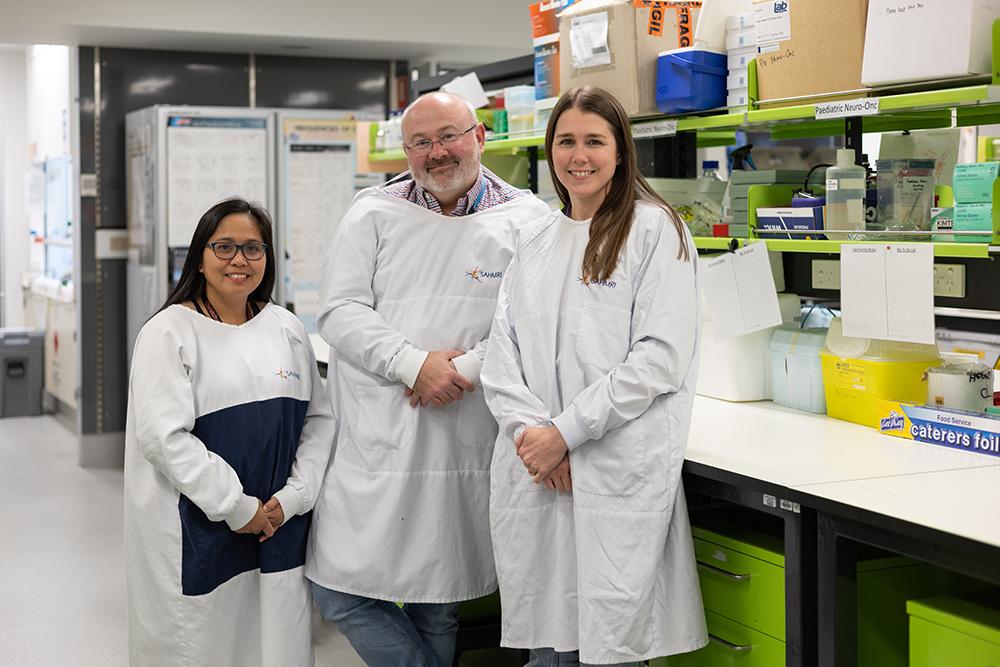
For Round 1 of 2025, the scholarship was proudly presented to two outstanding recipients, Rochelle Claude (pictured far left) and Amy Myatt (pictured second from left). Selected for their outstanding dedication to advancing burns care, Amy and Rochelle have been awarded the opportunity to attend the Australian and New Zealand Burn Association (ANZBA) Nursing Seminar, taking place in Hobart on May 30 – 31, 2025.
This opportunity, made possible through the BCM Scholarship, offers a valuable platform for nurses to expand their knowledge, share best practices, and further develop their expertise in burn injury management and care.
Looking ahead, the scholarship continues to pave the way for even greater opportunities. Round 2 of the 2025 BCM Scholarship will open soon, offering another chance for nurses to attend the ANZBA Annual Scientific Meeting held in Adelaide, between October 14 – 17, 2025.
Through the ongoing support provided by the Bridget Claire McCartan Scholarship, Bridget’s legacy lives on as a source of inspiration, empowerment, and excellence in the care of burns patients.